Recipient: Russell Aylsworth, 20 years old. Born in Hong Kong. World sailing ranking 62. Member of the Hong Kong Olympic Sailing team.

Medical report: Russell has several small radial tears in his right knee in the lateral meniscus. (refer radiologist’s report) His Sports Physiotherapist at the Hong Kong Sports Institute has suggested no surgery. His sports GP has also suggested no surgery. He will be seeing his orthopaedic doctor on Monday 18th May 2021 for a consultation . Should he say no surgery then we at Motion Dynamics will go ahead with a full knee rehabilitation program, 6 to 10 weeks of focused rehabilitation.
What is the Meniscus?
The meniscus are two C-shaped pieces of rubbery cartilage in the knee that fit between the femur (thigh bone) and tibia (shine bone). The meniscus act as shock absorbers and bumpers inside the knee joint. They allow the knee joint to glide smoothly and distribute the forces within the knee during activities such as walking, running, and jumping.
Meniscus Tear Causes and Symptoms
Meniscus tears come in many different shapes and sizes, and they can occur for a variety of reasons. Often times they occur as a result of a specific trauma such as landing awkwardly from a jump or being tackled in football. Other tears occur over time as a result of degeneration (wearing out) of the cartilage. In general, there are five common types of tears –flap, radial, vertical, bucket-handle, and degenerative. Each type has its own set of causes and treatment options.
In cases of traumatic tears, the patient often experiences an acute popping sensation in the knee followed by pain and swelling. In cases of degenerative tears, patients will sometimes experience the slow onset of symptoms. When a meniscus tear is symptomatic, a patient may experience pain, swelling, and/or mechanical symptoms (clicking, catching, and/or locking of the knee).
It is important to understand that each patient is different and the symptoms listed above do not always mean you have a meniscus tear. A diagnosis should be made by an orthopedic surgeon to ensure the injury is treated appropriately.
Diagnosis and Examination
Diagnosis is based on the patient history, physical exam, and imaging (such as X-rays and/or MRI). A meniscus tear can often be diagnosed on physical exam. The McMurray test is used to detect a tear of the meniscus, and will often cause pain and clicking when performed. Additional exam findings include swelling, pain with range of motion, and joint line tenderness. In most cases, x-rays of the knee will appear normal. If there is a concern about a meniscus tear or other knee injury, an MRI is usually performed. An MRI can be used to determine the size and shape of a tear as well as, look for other knee injuries such as cartilage or ligament tears.
Types of Meniscus Tears
The meniscus is a C-shaped structure that sits inside the knee joint. There are different types of meniscus tears and the type of tear can usually be determined with a knee MRI. Described here are 5 common types of meniscus tears.
- Radial Tear: Radial tears of the meniscus are the most common. These appear as small tears in the inner part of the meniscus. These tears occur in the avascular part of the meniscus (where there is no blood supply) and, as a result, have little ability to heal on their own..
Non-Surgical Treatment for Meniscus Tears
Surgery is not required in all patients with a meniscus tear. Your surgeon will take into consideration the tear type, as well as your specific lifestyle needs when determine the best treatment option. Non-operative treatment often includes a period of rest followed by a course of physical therapy. This allows the patient to build strength in the muscles surrounding the knee joint, allowing for normal knee function with activities. Nonsteroidal anti-inflammatory drugs (NSAIDs) may also be helpful in reducing pain and swelling. Lastly, some patients benefit from a corticosteroid injection into the knee. Corticosteroid is a strong anti-inflammatory and can often relive knee symptoms associated with a torn meniscus.
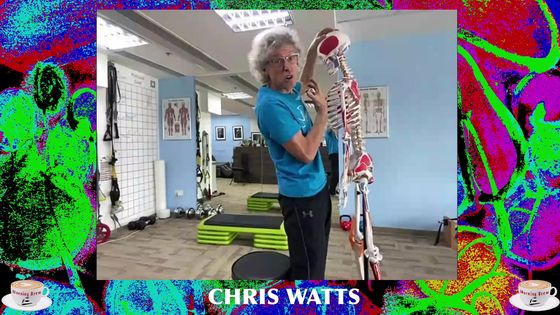
14th May 2021: Postural assessment with Chris Watts CEO Motion Dynamics Limited
Weight bearing assessment:
- Right hip up-slipped by 1.5 inches.
- Left side shoulder and hip torque (Twist) left to right by ¾ of an inch. Right shoulder elevated by 1 inch.
- Both shoulders internally rotated and protracted with left being more prominent in protraction.
- Right knee is externally rotated and laterally positioned. Tibial torsion on Right lower leg. Biceps femoris very restricted on the right side.
- 3 Inches of forward head protraction..
- Mild kyphosis in mid thoracic.
- Both SI joints are frozen mean no rotation or out-flaring and squish test is negative for mobility.
- Peroneal muscles on both ankles are weak.
Non-weight bearing postural assessment:
- Left hip upslip not right as when Russell was standing. Poor S I Joint mobility and no gliding of the joints on both sides.
- Right leg appears to be ½ inch shorter.
- Testing the psoas muscle on right side showed that it was severely hypertonic with pain up to 8 out of 10 when palpating. Left Psoas pain level 2 out of 10.
- Right quadricep is hypertonic and the right pelvis is anteriorly tilted by 10 degrees. Specifically the rectus femoris origin on the AIIS is also hypertonic with a 5 out of 10 pain scale on the trigger point of that origin.
- Hip external rotation whilst non-weightbearing is very noticeable compared to the left side. Piriformis on right side had less that 10 degrees of rotational motion out of a potential of 45 degrees.
- Both ankles are very inverted when non weight bearing. Weak evertors.
First Treatment: May 14th 2021
Objective report by Chris Watts-Motion Dynamics
Using Positional release therapy a technique designed to reduce tone in the muscles and joints on the Psoas and Iliacus as well as the upper quadriceps on the right side. Used a manual release technique to mobilise the Sacro-Illiac joints on both Illia. Did some sacral rocking and muscle energy work on the gliding action of the SI Joints.
We assessed Range of Motion on the hip joints. Both hip flexion and hip extension were limited. Right side single leg pelvic tilt was only 140 degrees out of a 160 degree potential and left was 150. Hip extension was zero degrees on both hips. Both psoas major and minor were hypertonic. To improve, Chris used the Active Isolated Stretching techniques with 3 sets on each side to loosen both hips.
Worked on distal hamstrings especially right side and insertions of the biceps femoris into the fibula. We had less than 45 degrees of full knee extension before experiencing sharp irritation to those insertion points on the fibula. Did 3 sets of active assisted stretching to open up the fascial sheaths that were over-shortened and thickened.
His hip/lumbo pelvic imbalances can and do create knee torsion and pressure on the meniscae. Russell was keen to see the link between the structural mechanics and functional bio-mechanics that causes excessive pressure on the tendons and joints.
Objective findings post treatment:
Russell has a straight shoulder, neck and hip alignment. His head is still 2 inches protracted, but his gait is softer and gliding with more fluidity. He was very happy with the session and we look forward to continuing with his spinal mobility and alignment next Thursday.
Session 1: May 14th 2021
Subjective findings from Russell Aylsworth
As an elite sailing athlete, strength and conditioning is a vital part of success. An often overlooked area in our training is recovery and mobility. Being in the gym five times a week is very stressful and demanding on the body.
In training, I tore my lateral meniscus in my right knee and decided to see Chris Watts at Motion Dynamics to help my recovery and fix my many other aches and pains through alignment training and postural and mechanical correction exercises.
When first seeing Chris, he did his examination on me with his laser eye vision seeing the errors in my posture, which surprised me to see how very accurate he was in spite of using an eyeball approach and no digital instruments and measurements. He did a very specific Range of Motion testing and joint restriction testing on the sacro-Illiac joints. We found out that I had a very tight hips, in extension and flexion and limited internal rotation on both hips.
To be honest, I didn’t think that my hips bothered me. But after doing his AIS stretching techniques and some manual soft tissue manipulations, I was surprised by how smooth and effortless it was to just walk around the room; I never knew I had this much potential to feel so loose and move so freely with my hips. After this first very enlightening session, I noticed a huge mobility gain for my sport enabling me to be even more fluid in my agility.
The day after the session with Chris, I was surprised how sore I was even though I was lying down for most of the session. The re-alignment of the fascial collagen fibres meant that I experienced some postural shifting and the utilisation of certain muscles that had become deficient from underuse.
I’m excited about next week’s session with Chris to see more improvements in my mobility and fluidity.
Session 2: May 20th 2021
Objective assessment from Chris Watts
Postural Re-assessment:
- Right shoulder protracted.
- Pec minor hypertonic and winging of right scapula.
- Serratus anterior right side weak and rhomboids under developed.
- Left hip upslip only 1/8 inch but causing mild functional lateral spinal flexion with head tilted mildly to right side.
- Anterior pelvic tilt more noticeable on right iIlium by 10 degrees.
- Both tibia’s are torqued outwards. Both Biceps femoris hamstrings are tight.
Treatment Plan and techniques

Strengthen the semi-tendinosis and inner thighs.
We spent the first part of the session on aligning the shoulders and removing the tension in the pec minor muscles.
Then used a special technique to stabilise the Rhomboid minor and major with 2 different angles of motion. Worked on stabilising the latissimus dorsi bi-laterally. This really helped with the shoulder and neck alignment.
Spent time on stretching the insertions of the bicep femoris on the lateral epicondyle of the fibula. Very restricted. Hips are more open today than last week. Finished with some upper back extensor stability work. Overall better awareness this week and better control of his mechanics.
Session 2: May 20th 2021
Subjective assessment from Russell Aylsworth
Milestones are always great to see. I love the process that I have with Chris because the first thing we do is examine my posture, and it was pleasing to know that I was generally more posturally aligned than last week. Chris determined that I have relatively underdeveloped rhomboids. Rhomboids are the back muscles that help keep the shoulder blades retracted as I have shoulders that roll forwards. I’ve been having upper back pain for a few months and have seen other physiotherapists, and they have never really gotten rid of the knot in my back that’s been nagging at me. I didn’t explain to Chris that I wanted to focus on this because I have gotten to the stage of just not caring about my nagging upper back pain. We started the session by aligning my shoulders and trying to release my very tight pectoral muscles. After releasing my pectoral muscles, the pain in my upper back just disappeared. It amazes me the potential my body has to be so loose and pain-free that Chris can see, and I would never realize without Chris’s help. Something I’ve never enjoyed doing is stretching because of the tingling pain and just makes time unbearably long.
Nevertheless, stretching is still essential for injury prevention and pain-free movement. Chris then worked on my hamstrings, which I have been told by a few physiotherapists and my gym coach that my hamstrings are very tight, but I can’t wait to see the improvement that we will have on them. Something interesting that Chris taught me was reworking my squat mechanics. We used a yoga ball on a wall to practice how my balance and posture are supposed to be while squatting, it felt entirely new for me and something I look forward to progressing. Overall I had an awesome session with Chris. The days after the session with Chris always feels like I’ve just gone to the gym, and it catches me off guard.
Session 3: May 28th 2021
Objective assessment by Chris Watts

Russell had a postural assessment that showed huge improvements to his head and neck alignment as well as hip alignment. No visible torque in the hips. Only right shoulder had a 1 inch right to left torque with shoulder internal rotation and protraction with some winging of the shoulder blade. Tibial torsion on both lower legs has somewhat improved especially on the left leg. The apex of the knee cap is finally straight. The Apex of the right knee is still turned out. Our objective is to work on the tibial rotators such as the biceps femoris and the popliteal muscles to balance out the pressure on the right knee. The ASIS the apex of the knee and the 2nd toe should all be in a straight alignment when standing and walking. There is some improvement on hip flexor mobility too. Right side still tighter than left.
Started to stabilise the upper back especially the rhomboids minor and major for better retraction of the shoulder blade.
Session 3, May 28th 2021
Subjective report by Russell Aylsworth
Chris and I had an excellent start to our session to support my overall growth to better alignment and healing. I had significant improvements in my head and upper body alignment. My hips still felt loose when I would walk, which was a satisfying feeling. My right shoulder was still slightly protracted forward, which I attribute to a challenging upper body gym session beforehand. We first worked on my shoulder mobility and just loosening up my shoulders. Chris mentioned that I still need to strengthen specific back muscles that have been hindering my posture. I was surprised that even though I think I’m training quite intensively, I’m still neglecting specific vital muscles for posture and feeling pain-free. It’s good to have someone like Chris aware of the muscle development expectations for your body personally.
Since the first session with Chris, my feet and my kneecaps are pointed outwards instead of straight on, which is how it should be. Helping fix my leg posture could potentially take the load off my right knee, which would help my meniscus tear recovery process. Chris went about this by stretching my very tight outer hamstrings and the other two parts of my hamstrings intensively. I think stretching is mentally more challenging to endure than actually lifting weights, so I always have to be relaxed every time Chris works on my legs. We finished off the session by strengthening my upper back muscles, specifically my rhomboids major and minor. Overall it was another solid session with Chris, and always so good to see such a significant improvement every week.
Session 4: May 31st 2021
Objective report by Chris Watts
On the weigh-bearing postural assessment, the pelvis was level in the mid-sagittal plane. However, the pelvis was still tilted forward by 5-10 degrees when measuring the alignment of the ASIS and PSIS. The hip flexors were very hypertonic on both sides especially the right side. For the first time I am able to see that the left and right knees are pointing straight forward. Only the right knee has the tendency to track laterally when walking. We did more pectoralis major and minor stretching which is getting much easier now. Both shoulders have a 60 degree horizontal abduction range, which is target athletic range for that specific movement. Only the internal shoulder rotation is limited . We are at 40 to 50 degrees of rotation and will need to build it to 90 degrees. The infraspinatus on both sides are weak.
Alvin Mesa who has a Master’s Degree in Physiotherapy and works alongside Chris Watts at Motion Dynamics did a series of tests on the right knee ligaments and meniscus. All the results were very functional with no pain or limitation or hypermobility associated with the knee. I believe we can start to do some gentle but focused stability work with the hip/leg and knee internal rotators. We started with the adductor stability program today.
Session 4: May 31st 2021
Subjective report from Russell Aylsworth
After my fourth session with Chris, I can say my meniscus tear is almost unnoticeable for my day-to-day life, and if I weren’t diagnosed or have MRI scans, I wouldn’t know I have an injury. A great indicator I have to attest to this is after my 21-day quarantine, I went indoor bouldering, and within 10 minutes, I could feel my right knee seize up, which caused me to stop climbing. Of course, no one likes to feel limited and forced to stop doing things they love. But after four thoughtful sessions with Chris, I was able to indoor boulder for an hour and a half with no issue on my knee. This is very encouraging to me for the potential our bodies have to recover with the guidance of Chris, of course.

This week’s fourth session with Chris was slightly different because I had the opportunity to work with Alvin Cruz, who holds a master’s degree in physiotherapy. The session was split, so I worked with Chris for the first half and Alvin for the second half. Chris started by stretching my pectoral muscles, which showed more flexibility than last week. During the pectoral stretches, I told Chris I had a knot on my upper trap muscle, and Chris knew how to relieve the pressure and work on my upper trapezoid immediately. He eased the tension by simply pushing up my upper trap for only ninety seconds to alleviate the discomfort I was feeling. In addition, Chris identified some muscles apart of my rotator cuffs were underdeveloped, which we will be working on moving forward to minimize the potential for injuries. We then worked on my very tight hip flexors and worked on my stride while walking. It was interesting and funny to learn how to walk again by activating my hip flexors while walking. I then was handed over to Alvin, who assessed my meniscus tear and did a series of tests to ensure that I didn’t have any issues with my ligaments alongside my tear. It gave me confidence when I could do tests like a single-leg pistol squat with relative ease. Alvin then began working on my fascial trigger points on my body and releasing built-up tension I would have got from a heavy gym load. Finally, Alvin spoke to me about how we should start doing knee stability work to regain some of the muscle around my knee joint to support it and hopefully aid recovery. I am very grateful to work with Chris and Alvin to help my body be at its best.
5th session: June 9th 2021
Objective report by Chris Watts
Alignment is significantly improved with all the mid-sagittal plane landmarks balanced. The only area that is still mildly imbalanced is the right shoulder girdle with a 1 inch shoulder protraction. Coronal plane shows a ½ inch forward head and a mild kyphotic T6-T9 curve. Also the right ilium is 10 degrees anteriorly tilted whilst the left ilium is 5 degrees anteriorly tilted.
We began the session with deep psoas and illiacus stretching using the AIS active dynamic stretch techniques which engages the Gluteus maximus medial fibres to extend the hip. We are now able to reach 10-15 degrees of hyperextension on both sides of the hip. This is very different to our first session where we were only able to reach zero degrees of hip extension.
We spent more time on centralising the right patella which is still mildly turned out. We performed 3 sets of outer hamstring (biceps femoris) stretches on both sides. We were able to reach 100 degrees of single leg lifts. This represents full functional ROM for the hamstrings with a locked out knee. Russell also had some DOMS from training the distal hamstrings at the Sports institute that made the stretching more challenging. We landed up doing 3 sets of 12 repetitions on both sides.
We spent 10 minutes releasing the right pectoralis major and minor using Neuromuscular and myofascial release techniques and finished the session with more stability training of the upper back and the shoulder external rotators using the “shoulder-cizer” device.
We have one more training session next week. So far the right meniscus and right knee pain is minimal and barely noticeable, not causing any significant slowing down of his general fitness training.
Session 5: June 9th 2021
Subjective report by Russell Aylsworth
Today was the first session with Chris, where my posture was almost entirely aligned except for my right shoulder, which rides forward a little. From an athlete’s perspective, working with Chris has made my body considerably loose. I anecdotally feel that I’ve been able to lift heavier weights in the gym and recover better. Chris and I started our session by working on leg extensions. Even though I did not realize it, Chris saw an improvement in the range I could get; it was motivating to see how much my body can adapt and become healthier with Chris’s help. My hamstrings have always been tight, and when I would see the sports massage people at Sports Institute, and they would always struggle to loosen my hamstrings. Chris is a very determined character and pushes my body to the potential he’s very aware of, and Chris and I work with my awfully tight hamstrings to lengthen them. It was extra tricky this session, especially to work on my hamstrings because I’ve had a gym session just before seeing Chris, yet Chris doesn’t lose confidence in what he does, and we push through together. By the end of the session, we worked on loosening my pectoral muscles from the strenuous effort I put through them from doing some bench presses earlier in that day. After every session with Chris, I always feel light under my feet and just more lively. Doctors have told me that with the type of meniscus tear I have, there is no blood flow going to the Injury, so my meniscus tear will never heal on its own. When I first told Chris about my meniscus tear before I started working with him. He had complete faith and confidence he could help me. It’s fantastic to know someone like Chris who’s invested in who you are and wants the best for you. Since working with Chris, I’ve been pain-free in my right knee and been able to go back and do the sports I love to do and improve and become a better, stronger athlete.
6thand final session: June 17th 2021
Objective report by Chris Watts

Assess, Address and Reassess is how we always go through our sessions here at Motion Dynamics.
The postural assessment on Russell showed a ¼ inch elevation to the left shoulder, a ¼ inch
depression of the right occiput and zygomatic arch. The right Illium was anteriorly tilted by 5 degrees only but caused some discomfort in the hips. Russell was unable to note exactly where that discomfort was but he did complain of some upper to mid back irritation.
We started the session with a series of deep AIS stretches of the right Psoas and illiacus. I then showed him how to release those muscles with a self-stretch technique. I noticed that after working on the psoas his right knee which has the radial tears in the meniscus had totally centred so that the apex of the knee cap was pointing directly forward even when he was walking. We did some Rhomboid minor and major stability work to draw back the shoulders 5 degrees. Now the distance between the vertebral border of the scapulae and the spinous processes is around 1.5 inches. For the right shoulder external rotators we were side-lying and used 4kgs for s set of 10 reps and then 5kgs for 10 reps followed by 6kgs at 10 reps. We were at maximum capacity for those shoulder external rotators on the right side.
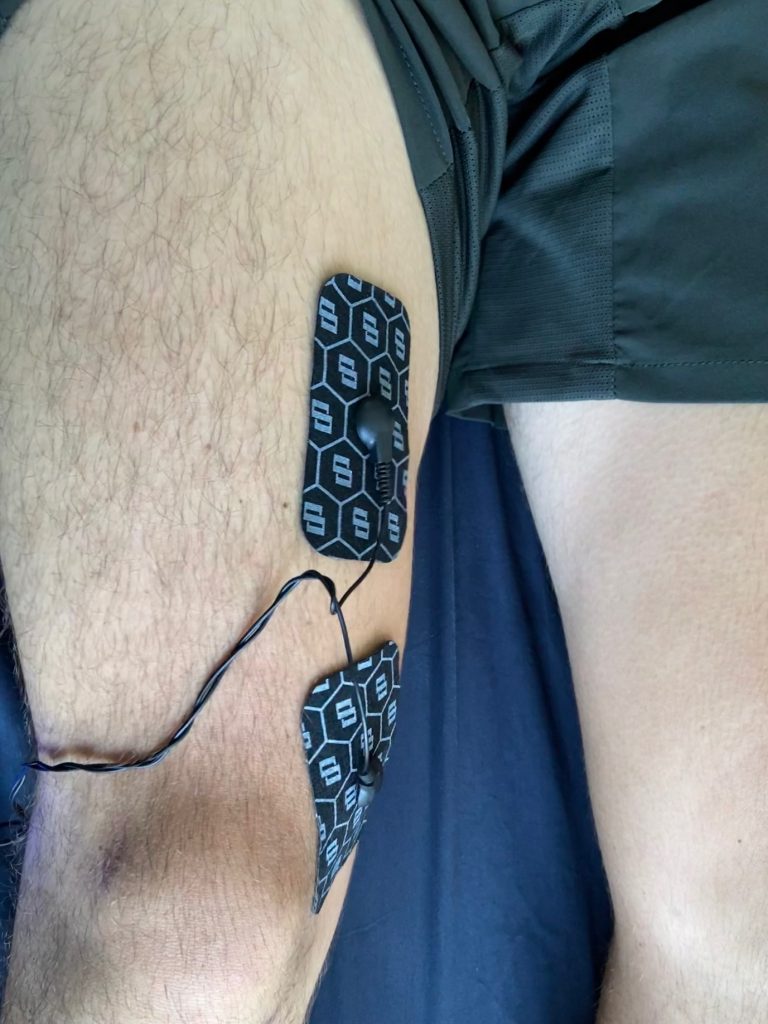
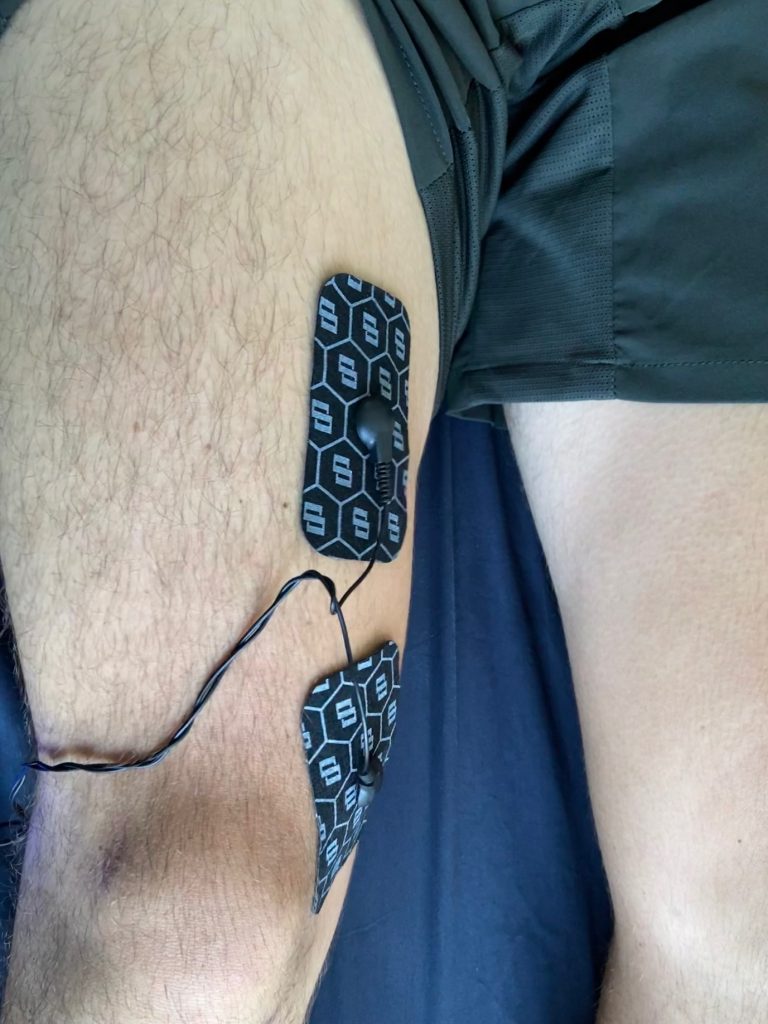
The shoulder seems to be more naturally retracted and pinned back on the right. We took photographs of Russell’s posture at the end of the session and his knees when standing and walking to highlight the new centralised position. We also used a Swiss “Dipulse” EMS device to stimulate the Vastus Medialis Obliquus on the right thigh. It was very red and very pumped after using 50 hertz and intensity of 32 for 27 minutes.
I recommend that he supplements his training at the Sports Institute with an EMS device for the inner thigh muscles.
6th session: June 17th 2021
Subjective report from Russell Aylsworth
Bittersweet to come to an end of my sessions with Chris and his team at Motion Dynamics. For the past six weeks, I have felt a considerable improvement in my overall posture and just the fluidity I have taken for granted. Being 20, I definitely underestimated how free and lose my body could actually be and never really knew thoroughly the potential my body has to adjust to the new postural alignment. Being very rigorous in the gym, I have neglected certain parts of my recovery. As an elite athlete, I would consider myself a healthy individual who is aware and attentive to my body’s needs. Chris has considerably widened my scope and awareness of the potential my body has to be optimal, and anecdotally I have found my strength and form to improve each session I have in the gym, which is huge and rewarding to see. Chris’s timing was quite good because we did not have anything serious to work on for our final session together.
Today was more of maintaining and providing me with exercise and stretches I could do at home before he sends me off. We did work on strengthening some of my weaker back muscles, such as the Rhomboid minor and major. I told Chris about this knee extension test which compares the strength of my quadriceps and hamstrings. The ratio of quadriceps strength to hamstring strength can help indicate future ACL tears. For myself, because I tore my right meniscus, my inner thigh muscles on my right leg were significantly weaker than my left leg, even though I am right-handed. A neat machine Chris wanted to try the Di-Pulse a Swiss EMS device that sends electric shocks specifically to the muscle to stimulate stress like in the gym. What I found was fascinating about the device was the accuracy it had on my specific muscle. Even though I was lying down in a relaxed position, this specific muscle in my leg was still working. Days after using this EMS Device, that specific muscle had the same soreness from a traditional gym workout.
After my final session with Chris, I was planning on going sailing for the first time in 2 months to see how my knee would fair. Even without surgery and just training my knee and the help I got from Chris has given me no trouble whatsoever, and I wouldn’t be able to tell I had an injury, to begin with. Chris’s warmth and genuine care for his clients are rare to see, and the adaptability matched with his understanding of the complexities of the body is honestly quite fantastic to see and further my knowledge. The type of care I received from Chris is exceptional even though I have exclusive access to the Hong Kong Sports Institution. Chris ‘ attention to the detail ensured that my Postural fitness will stay with me for a very long time. Thank you so much, Chris, for the opportunity to work with you, and helping me along my journey as an athlete is a great experience.
Case study written by Chris Watts- founder and CEO of Motion Dynamics
www.motiondynamics.hk
Tel: +852 28823397